Mpox: What You Need to Know

Mpox’s Origin
Mpox is a viral disease that is caused by infection with monkeypox virus. It is an emerging zoonotic disease caused by the monkeypox virus (MPXV), a member of the Orthopoxvirus genus in the Poxviridae family, which also includes cowpox, horsepox, smallpox (variola), and vaccinia viruses.
MPXV is endemic in parts of Central and West Africa, where two distinct clades of MPXV, Clade I (formerly Congo Basin clade) and Clade II (formerly West African Clade), circulate in different geographical regions. Prior to 2022, the main geographic risk area of endemic mpox transmission has been in Africa, where animal-to-human transmission may occur from close contact with infected animals, preparation of bush meat, or direct contact with contaminated tissues and bodily fluids.
Symptom-presentation of both genetically distinct variants of monkeypox virus – Central (Clade I) and West Africa (Clade II ) are indistinguishable.
Human infections with the West African clade appear to cause less severe disease compared to the Congo Basin clade.
2022-2023 global outbreak of MPXV Clade II
Since May 2022, an mpox outbreak of MPXV Clade II began to occur on an international scale representing the first known instance of sustained transmission chains in countries without direct or immediate epidemiological links to areas of West or Central Africa.
Human infections of Clade II remain mostly driven by sexual transmission, primarily in the high-risk groups including men who have sex with men (MSM).
The WHO has assessed the global risk for mpox Clade II to be moderate.
Ongoing outbreak of MPXV Clade I in the DRC (2023-2024)
It was also reported that since 2023, there has been an increase in the number of MPXV Clade I cases reported by the DRC. The outbreak had spread to previously unaffected provinces and into urban settings driven by sexual and non-sexual direct contact.
Since July 2024, at least five other countries in the region, including those where MPXV Clade I was not endemic, have also reported mpox cases and outbreaks. The current upsurge of MPXV Clade I in parts of Central and East Africa and the cross-border spread is concerning as MPXV Clade I is known to cause more severe disease.
On 14 August 2024, the World Health Organisation (WHO) declared that the mpox outbreak in the Democratic Republic of the Congo (DRC) and a growing number of countries in Africa constituted a Public Health Emergency of International Concern (PHEIC).
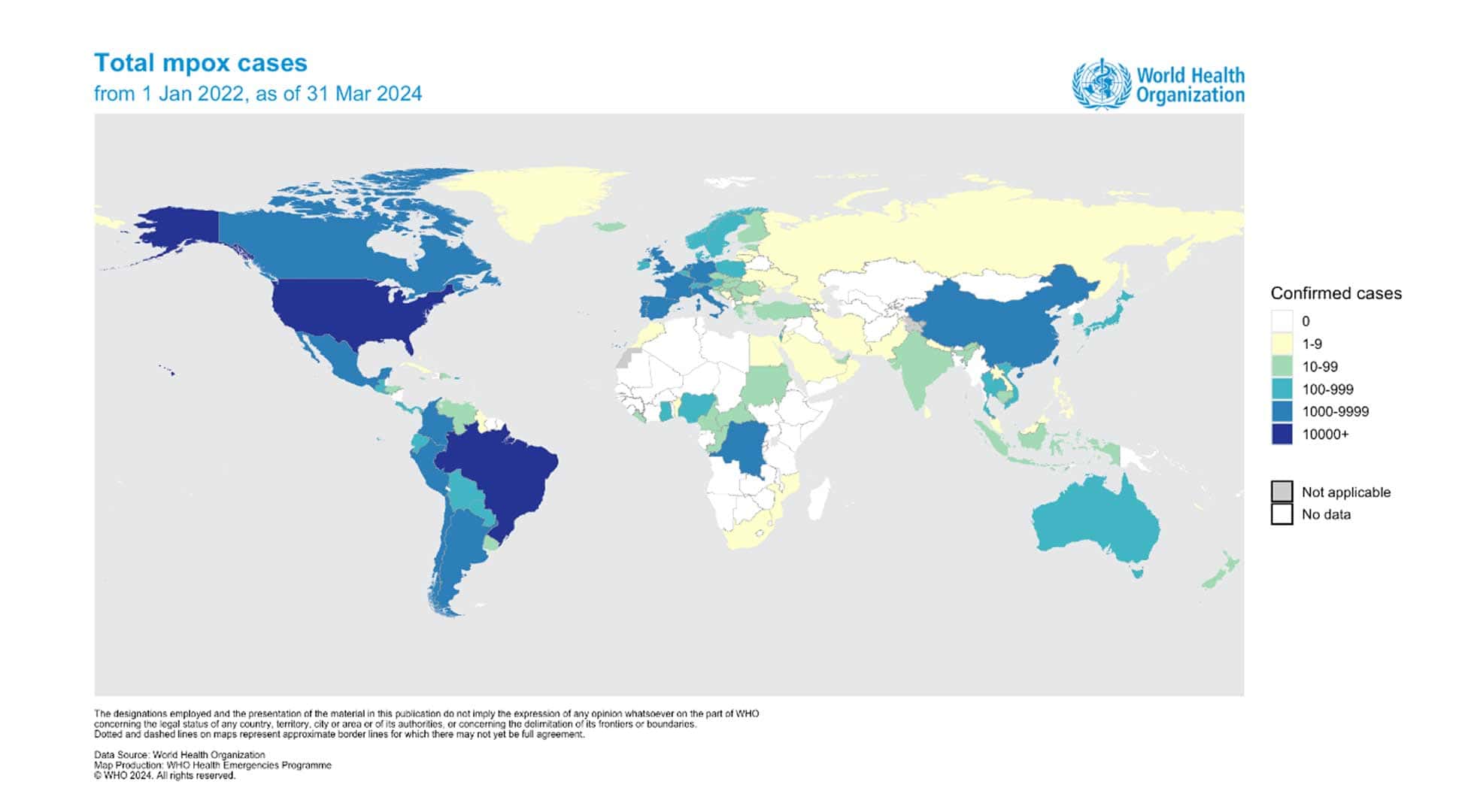
Current global situation
As of 30 September 2024, over 31,000 cases of mpox, including 860 deaths (case fatality rate of around 3 per cent), have been reported in 2024, as part of the ongoing MPXV Clade I outbreak in the DRC and in neighbouring non-endemic African countries such as Burundi, Kenya, Rwanda, and Uganda. In addition, resurgences in mpox cases linked to both MPXV Clade I and Clade II have been detected in other endemic African countries in 2024.
Outside of Africa, MPXV Clade Ib has only been detected in Sweden, Thailand, and India, which have each reported one case among travellers since August 2024, but have not led to further spread among the locals.
The WHO has assessed the risk of spread of MPXV Clade I, with potentially more severe consequences to be high within the DRC, while the global risk for countries with historical or no prior infections remains moderate.
In Singapore
As of October 2024, there were 16 cases of mpox detected compared to 21 cases in 2023, with the Ministry of Health (MOH) confirming that all cases in Singapore have been of the milder Clade II strain.
MOH added the immediate public health risk to the country is low and that precautionary measures are in place.
How mpox is transmitted
Transmission occurs when a person comes into close contact with the virus through an infected animal, infected person or contaminated materials and environment.
Animal-to-human transmission may occur via:
- Bite or scratch from an infected animal
- Bush meat preparation
- Direct contact with the blood, body fluids, skin, or mucosal lesions of infected animals
Human-to-human transmission is limited but can occur via:
- Prolonged exposure to respiratory droplets
- Direct physical contact with the blood, body fluid, or skin rash from infected individual or contaminated materials

Image credit: www.who.int
Symptoms of mpox
The incubation period of mpox is about three to 21 days after exposure. Early symptoms are non-specific and include:
- Fever and chills
- Headache, muscle aches
- Swollen lymph nodes
- Intense lack of energy
Within one to three days after the onset of fever, an infected person develops a rash; often starting from the face before spreading to other parts of the body, especially the palms and soles for most cases. The rash progresses uniformly to become fluid-filled vesicles and then pustules, before crusting occurs in approximately 10 days before falling off. Most infections with MPXV were mild and self-limiting with symptoms lasting from two to four weeks.
|
|
|
|---|---|---|
|
|
|
While MPXV Clade I have historically been characterised by more severe disease and higher mortality than Clade II infections, clinical presentations of both clades are indistinguishable. Serious complications or death can occur in vulnerable persons (e.g. pregnant women, young children, or immunocompromised individuals).
An infected person is contagious from onset of fever until the skin lesions have scabbed over.
MOH’s definition of a suspect case
An individual who presents with:
a. Unexplained acute rash;
AND
b. One or more accompanying symptoms (including fever, headache, backache, swollen lymph nodes, generalised weakness);
AND
c. Within the last 21 days prior to onset of illness had one of the following exposures:
-
- Had a travel history to areas or regions with reported confirmed case of mpox.
- Had a history of *close contact with an infected person(s).
- Had a history of sexual or intimate in-person contact with persons in a social or sexual network experiencing mpox activity (including men who have sex with men (MSM) and commercial sex workers) and presents with lesions on or near the possible route(s) of exposure during the sexual activity (e.g genitals, anus, oral or hand regions).
*Close contact is defined as (i) being within two metres of an infected person for at least 30 minutes, (ii) having physical contact with an infected person, or (iii) having physical contact with contaminated surfaces or materials, such as clothes or bedding contaminated with bodily fluids and scabs.
How mpox is diagnosed
Detection of viral DNA by polymerase chain reaction (PCR) is the preferred laboratory test for mpox. The best diagnostic specimens are directly from the rash – skin, fluid or crusts, or biopsy where feasible. In the absence of skin lesions, testing can be done on oropharyngeal, anal, or rectal swabs.
Blood testing is not recommended, and asymptomatic contacts do not require testing.
Treatment for mpox
Mpox is typically a self-limiting illness, with symptoms usually resolving spontaneously within 14 to 21 days. Treatment is typically symptomatic and supportive.
As children under 16 may be at higher risk for severe disease and death if infected with mpox, consultation with a paediatric infectious disease specialist is recommended.
Mpox infection during pregnancy may result in pregnancy complications, stillbirth, or congenital mpox infection. Consultation with obstetrics and infectious disease specialists is recommended.
De-isolation of ill contacts should be done only when:
- No new rashes have developed for at least 48 hours.
- All rashes have crusted over, all scabs have dropped off, with fresh intact skin underneath.
There is no requirement for laboratory testing such as blood, urine, or throat PCR testing prior to de-isolation.
Complications
The disease is usually self-limiting, with most patients recovering within two to three weeks.
However, in some cases the virus can cause serious complications such as pneumonia, sepsis (blood infection), encephalitis (brain inflammation), and eye infection with ensuing loss of vision.
Newborns, children, and people with underlying immune deficiencies are at higher risk of severe complications and death.
MPXV Clade I is known to cause more severe disease (recorded case fatality rate of about 3 to 4 per cent in the DRC) than the MPXV Clade II (case fatality rate of about 0.2 per cent).
Prevention
| Maintain a high standard of personal hygiene, including frequent hand washing after going to the toilet, or when hands are If water is not available, use an alcohol-based hand sanitiser that contains at least 60 per cent of alcohol. | |
| Avoid direct contact with skin lesions of infected living or dead persons or animals, as well as objects that may have become contaminated with infectious fluids, such as soiled clothing or linens (e.g bedding or towels) used by an infected person. | |
| Avoid sharing common items that may be contaminated with bodily fluids. | |
| Put on a mask to prevent inhaling infected respiratory droplets if you are caring for an infected person or in prolonged, close proximity to ill contacts. | |
| Avoid contact with wild animals that could harbour the virus, and consumption of bush meat. | |
| Practise safe sex, including avoiding high-risk sexual activities such as having multiple sex partners or engaging in casual sex. | |
| As a precaution after recovery from mpox, the WHO recommends the use of condoms consistently during sexual activity (receptive or insertive oral / anal / vaginal) for at least 12 weeks to reduce the potential for transmission of mpox. This is recommended in view of the fact that viral DNA has been detected in seminal fluid of mpox-infected individuals. | |
| Returning travellers, especially from areas affected by mpox should seek immediate medical attention if they develop any disease symptoms (e.g sudden onset of high fever, swollen lymph nodes, and rash) within three weeks of their return. They should call the clinic ahead of their visit, so that special precautions can be taken to protect others. They must inform their doctor of their recent travel history. | |
| Vaccination – the MVA-BN (JYNNEOS) vaccine is a live but non-replicating, third-generation smallpox vaccine, which has efficacy in preventing smallpox, mpox, vaccinia, and other orthopoxvirus infections. While JYNNEOS is estimated to provide over 80 per cent protection against mpox, current data remains limited in concluding the level and duration of protection conferred by vaccination. The vaccine consists of two doses, given 28 days apart, and is approved by US FDA for prevention of smallpox and mpox in adults 18 years and older. Since August 9, 2022, JYNNEOS has been authorised by US FDA for people aged <18 years old.It may be recommended for certain high-risk groups such as: |
|
|
|
| In line with international recommendations, mass population-wide vaccination is currently not recommended as a preventive strategy for mpox, as the risk to the general public remains low with disease transmission predominantly via close physical or prolonged contact. |
|
| Areas exposed to mpox cases should be terminally cleaned with bleach-based disinfectants (i.e. 5000ppm). This can be prepared by diluting 1-part common household bleach (5 per cent sodium hypochlorite) with nine parts of water. |
When to seek medical attention and what precautions to take
Returning travellers from areas affected by mpox should seek medical attention should they develop a sudden onset of high fever, swollen lymph nodes, malaise, headache and rash within three weeks of their return.
They should call the clinic ahead of their visit, so that special precautions can be taken to protect others. They must inform their doctor of their recent travel history.
To minimise any potential spread, they should also cover any rashes, wear a well-fitting mask and avoid physical contact with others.
References:
- MOH Circular No 02/2023; 55A/2024
- JOINT MOH-NCID GUIDANCE FOR MPOX FOR HEALTHCARE PROFESSIONALS (GENERAL PRACTITIONERS) – 16 May 2023
- https://www.who.int/news-room/fact-sheets/detail/monkeypox
- https://www.cdc.gov/poxvirus/mpox/outbreak/index.html









